Understanding Ankylosing Spondylitis: Early Signs and Diagnosis
Ankylosing spondylitis affects approximately 0.1% to 0.5% of the adult population worldwide, with a higher prevalence in certain genetic groups. According to the Spondylitis Association of America, this condition often goes undiagnosed for years, leading to prolonged discomfort and complications. Early detection and diagnosis are crucial to managing the symptoms effectively and improving the quality of life for those affected. This blog aims to provide an overview of ankylosing spondylitis, its early signs, and the methods used for diagnosis and treatment.
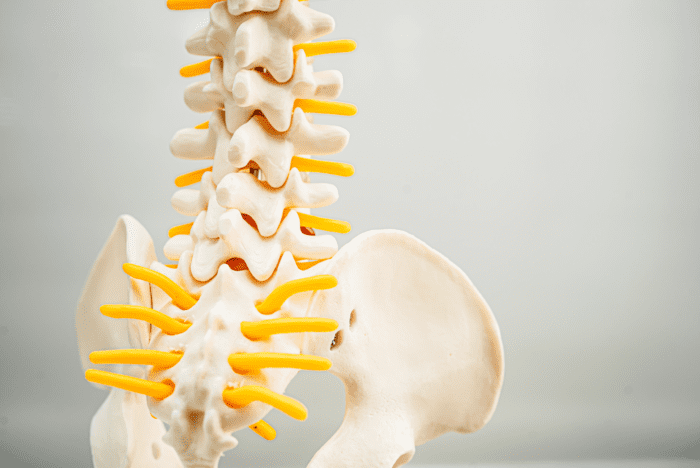
What is Ankylosing Spondylitis?
Ankylosing spondylitis is a type of arthritis that predominantly impacts the spine, though it can affect other joints and organs. It causes inflammation of the vertebrae, which can lead to chronic pain and stiffness. In severe cases, this inflammation can result in the fusion of the vertebrae, a condition known as ankylosis, which significantly reduces flexibility and mobility.
Early Signs of Ankylosing Spondylitis
Identifying the early signs of ankylosing spondylitis is vital for timely intervention. Some of the initial symptoms include:
Chronic Back Pain
Persistent pain and stiffness in the lower back and hips, especially after periods of inactivity or in the morning.
Improvement with Exercise
Unlike other types of back pain, the discomfort associated with AS often improves with physical activity and worsens with rest.
Pain in Other Joints
Inflammation can also occur in other parts of the body, such as the shoulders, knees, and feet.
Fatigue
Persistent tiredness and a general feeling of malaise.
Eye Inflammation
Uveitis or iritis, which is characterized by red, painful eyes and blurred vision, can also be an early indicator of AS.
Diagnosis of Ankylosing Spondylitis
Diagnosing ankylosing spondylitis involves a combination of medical history, physical examination, and diagnostic tests:
Medical History and Physical Exam
A thorough review of symptoms and family history of AS or related conditions.
Imaging Tests
X-rays and MRI scans are used to detect changes in the sacroiliac joints and spine. Early changes may be subtle, so MRIs can be more effective in the initial stages.
Blood Tests
These tests can help identify markers of inflammation and the presence of the HLA-B27 gene, which is commonly associated with AS.
Treatment of Ankylosing Spondylitis
While there is no cure for ankylosing spondylitis, several treatment options can help manage the symptoms and slow disease progression:
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) are typically the first line of treatment. In more severe cases, biologics and disease-modifying antirheumatic drugs (DMARDs) may be prescribed.
Physical Therapy
Regular exercises and stretches are designed to maintain flexibility and posture.
Lifestyle Modifications
Maintaining a healthy weight, quitting smoking, and engaging in low-impact exercises like swimming or yoga.
Surgery
In rare cases, surgery may be necessary to repair significant joint damage or correct severe spinal deformities.
Why Choose FirstChoice Rheumatology
Recognizing the early signs of ankylosing spondylitis and obtaining a prompt and accurate diagnosis is essential for managing this chronic condition effectively. At First Choice Rheumatology, we are committed to providing comprehensive care and prompt services to our patients. Our experienced team of rheumatologists utilizes state-of-the-art diagnostic tools and personalized treatment plans to address the unique needs of each individual. With a focus on patient education, ongoing support, and advanced therapeutic options, First Choice Rheumatology ensures that you receive the highest quality of care to manage ankylosing spondylitis and improve your quality of life. If you are experiencing symptoms or have concerns about AS, don't hesitate to reach out to us for expert consultation and timely intervention. Contact us.
FAQs
1. What are the common symptoms of ankylosing spondylitis?
The common symptoms of ankylosing spondylitis include chronic back pain and stiffness, particularly in the lower back and hips, which worsen with rest and improve with activity. Other symptoms can include pain and swelling in other joints, fatigue, and eye inflammation.
2. How is ankylosing spondylitis diagnosed?
Ankylosing spondylitis is diagnosed through a combination of medical history, physical examination, imaging tests like X-rays and MRIs, and blood tests to detect markers of inflammation and the HLA-B27 gene.
3. Can ankylosing spondylitis be cured?
Currently, there is no cure for ankylosing spondylitis. However, treatment options such as medications, physical therapy, and lifestyle modifications can help manage symptoms and slow disease progression.
4. What lifestyle changes can help manage ankylosing spondylitis?
Lifestyle changes that can help manage ankylosing spondylitis include maintaining a healthy weight, engaging in regular low-impact exercises like swimming and yoga, quitting smoking, and practicing good posture techniques.
Understanding ankylosing spondylitis and recognizing its early signs can lead to timely diagnosis and effective management, improving the overall well-being of those affected by this chronic condition.
About Dr. Shalene Badhan

When it comes to managing rheumatologic conditions, empathy is as crucial as expertise. Dr. Shalene Badhan, our lead Rheumatologist and an Internal Medicine specialist, embodies both. Having been diagnosed with psoriasis and psoriatic arthritis herself, Dr. Badhan brings a unique perspective to her practice, combining professional excellence with personal insight. Her journey through diagnosis, treatment, and daily management of autoimmune diseases allows her to connect with her patients on a profound level, offering not just medical advice but also understanding and solidarity.

